New Research: How Stress Affects Inflammation, Neurodegeneration, the Gut Microbiome, Cancer Treatment and Relationships

Stress is a particular passion of mine. I love learning how to reduce negative stress, and I’m fascinated by the ways stress affects our health.
We do not know everything there is to know about stress. In the grand scheme of things, scientists are only beginning to understand the myriad ways in which chronic stress affects us, and significant discoveries are being made every year. In this post, I’ll discuss recent research on these topics:
-
Stress damages mitochondria, leading to disease and aging.
-
Stress causes glucocorticoid receptor resistance, increasing inflammation.
-
Stress changes neural connections, decreases brain volume, and contributes to Alzheimer’s disease.
-
Stress changes the composition and behavior of gut bacteria and causes “leaky gut.”
-
Stress increases metastasis and decreases the efficacy of cancer treatment.
-
Stress is contagious at a cellular level.
Stress and the Mitochondria
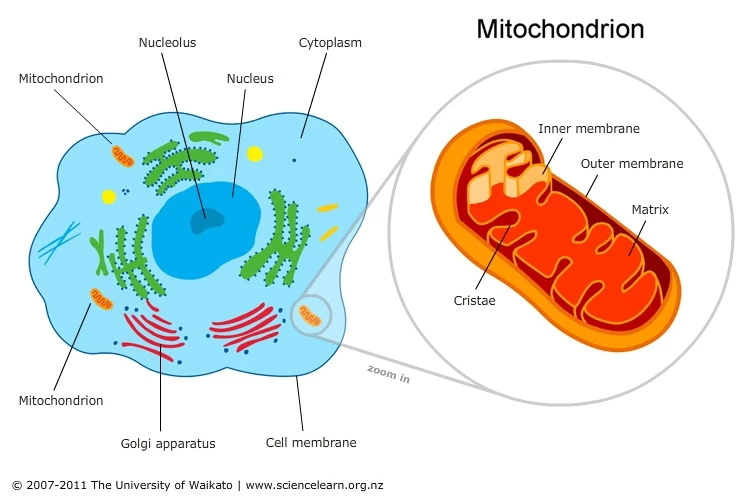
Mitochondria translate psychological stress into disease and aging—providing biological proof of the mind-body connection. Mitochondria are organelles (subunits of cells) found in most cells of our body. The most important roles of mitochondria are to produce energy for cells, regulate cellular metabolism, and send signals to other cells. When mitochondria aren’t functioning as they should, severe diseases involving many different bodily systems can result.
A revealing 2018 review (1) describes how acute and chronic stress affects mitochondrial structure and function, especially in the brain. These changes can then lead to inflammation throughout the body, increasing the risk of many inflammatory diseases. It’s believed that mitochondria play a role in regulating our physiological stress response, so stress-induced changes in mitochondria may result in even more stress. In addition, mitochondria have their own DNA, and damage to mitochondrial DNA caused by stress speeds up aging in mammals.
Evidence shows (2) that mitochondria “sense, integrate, and signal information about their environment.” The growing body of evidence demonstrating how mitochondria translate stress into disease is exciting for the field of psychosomatic medicine because it provides biological proof of how the mind and body interact.
Stress and Glucocorticoid Receptor Resistance
Chronic stress leads to glucocorticoid receptor resistance and increased inflammation. When we perceive stress, a series of hormones released in the brain triggers the adrenal gland to secrete hormones called glucocorticoids. These bind to glucocorticoid receptors, which are present in almost every cell in our body. Glucocorticoids play a critical role in regulating our stress response, including how much inflammation occurs.
Glucocorticoids must be able to bind to their receptors to do their job. Research now shows (3) that chronic stress leads to glucocorticoid receptor resistance, making it difficult or impossible for glucocorticoids to bind. This resistance causes our inflammatory response to be longer and/or more intense, and our risk for suffering from the common cold, asthma, autoimmune diseases, cardiovascular disease, type 2 diabetes, and other inflammatory conditions is increased.
Stress and the Brain
Researchers from Zurich, Switzerland, were surprised and excited by what they discovered (4) about how stress changes the brain in a 2019 study published in Neuron. (5)
When we perceive a threat, the neurotransmitter noradrenaline (aka norepinephrine) is released. Previous research has suggested that noradrenaline probably facilitates connections between parts of the brain.
The research team from Zurich manipulated the brains of mice so that they could control when noradrenaline was released. They found that noradrenaline instantly “rewired” the mouse brains, making actual structural changes to neural connections. This finding suggests that the long-term effects of stress on the brain may be more profound than previously thought.
In the study, the most significant structural changes occurred in areas of the brain that process sensory information (like what we see and hear) and in the amygdala. The amygdala is a cluster of nuclei in the limbic system that plays an important role in the emotional responses of fear, anxiety, and aggression, as well as in-memory and decision making. The amygdala is typically overactive in people with stress-related conditions, including anxiety and depression.
Chronic stress affects the amygdala by another means as well. Prolonged high levels of glucocorticoids stimulate neuron growth in the amygdala and make synapses more active and sensitive.
Stress and the release of glucocorticoids have also been shown to hardwire neural connections between the hippocampus and the amygdala, potentially creating a cycle in which the brain becomes stuck in a constant state of stress.

Of equal concern is the fact that the effect that chronic stress has on decreasing brain volume and connectivity. Data from 2,231 participants in the Framingham Heart Study (6) shows that people with increased levels of cortisol (one of the glucocorticoids) experience brain shrinkage and memory loss.
And a study of 103 healthy subjects (7) showed decreased brain volume in the medial prefrontal cortex and the insula in people who had experienced repeated exposure to stress as well as those who had only experienced a recent stressful event. The affected areas of the brain regulate emotions, stress, reward regulation, memory, decision-making, and impulse control. The study authors suggest that this decrease in brain matter may help to explain the connection between stressful life events and an increased risk of depression, addiction, and other stress-related disorders.
Glucocorticoids have also been shown to decrease the volume of the hippocampus (8), a part of the brain involved in memory, learning, attention, and ironically, regulating glucocorticoid secretion. So the more stress you experience and the more damage is done to your hippocampus, the less effective it is at regulating glucocorticoid levels, and the more glucocorticoids build up in your system. This is a vicious cycle that can make it difficult to reduce your level of stress.
There is a growing body of research on how stress contributes to Alzheimer’s disease. Based on current research (9), stress increases the expression of Amyloid Precursor Protein (APP) and the production of Aβ peptide, which then gets deposited into amyloid plaques. Amyloid plaques trigger an inflammatory response in the brain, (10) and it’s believed that neurotoxic inflammatory substances contribute to the neurodegeneration that occurs in Alzheimer’s. Stress also elevates levels of the tau protein, which leads to neurofibrillary tangle formation and neurodegeneration.
Stress and Your Microbiome
Stress changes the composition and behavior of gut bacteria and causes “leaky gut.” The human microbiome (11) describes the trillions of microorganisms (aka microbiota or microbes) that reside within our bodies. Our gut microbiome has been getting a lot of attention lately because of the discoveries researchers have made about how our gut microbiome affects our overall health. These discoveries have led to a booming market for pre- and probiotics that claim to improve our gut health.
There is “bidirectional cross-talk” between our gut and our brain. Our enteric nervous system (aka ENS; the network of 200-600 million neurons in our digestive system) communicates with our central nervous system (CNS) in many ways, including via the vagus and pelvic nerves and systemically via immune system cells. The cross-communication between our digestive system and our brain means that there is a high rate of comorbidity of gastrointestinal and psychiatric disorders. For example, up to 94% of people with irritable bowel syndrome (12) also suffer from a psychiatric disorder.
A 2019 study (13) shows that social stress changes both the composition and the behavior of gut bacteria. After subjecting mice to repeated stress, the mice had significant differences in their gut bacteria, most notably in two types of bacteria linked to multiple sclerosis in humans. And in the stressed mice, some gut bacteria turned into destructive pathogens that are likely to infect tissue, trigger the immune response, and lead to autoimmune conditions.
Several studies show how psychological stress increases gut permeability (aka “leaky gut”), a condition in which bacteria and toxins are able to leak through the intestinal wall, causing a wide variety of health problems.
We’re only beginning to understand the vast ways in which stress affects our gut microbiome (14) and vice versa. To learn more about this topic, check out The Mind-Gut Connection by Dr. Emeran Mayer.

Stress and Cancer
Stress increases metastasis and decreases the efficacy of cancer treatment. A healthy immune system is our number one line of defense against cancer. Unfortunately, a 2017 study (15) showed that chronic stress suppresses the immune system’s response to cancer and reduces the efficacy of immunotherapy treatments. The researchers suggest that improving immune system function may improve the rate of success of conventional therapies like chemotherapy as well because many of these therapies rely on the immune system for their efficacy. The researchers stated that “there is now pre-clinical evidence to suggest that treatments and lifestyle interventions to manage or reduce stress levels will improve the chances of these patients responding to therapies.”
A 2019 study (16) made two important discoveries about how stress hormones affect breast cancer metastasis and treatment. First, the study showed that increased levels of stress hormones led to increased colonization (growth in secondary locations) and heterogeneity (diversity) of cancer cells—both of which make cancer more difficult to treat and decrease the survival rate of the patient.
Second, the study showed (17) that synthetic derivatives of stress hormones (corticosteroids), which are often used as anti-inflammatories in cancer treatment, actually decrease the efficacy of chemotherapy. This finding suggests that corticosteroids should be used with caution in cancer therapy. One of the researchers, Mohamed Bentires-Alj, states that “These findings highlight the importance of stress management in patients…Moderate exercise and relaxation techniques have been shown to correlate with enhanced quality of life and greater survival in patients.”
Stress and Our Cells
Stress is contagious at a cellular level. If you have a family member, friend, or romantic partner who is always stressed out, you may have noticed the effect their stress has on you. You may feel that you “absorb” their stress or that you can’t relax around them. Well, scientists have now discovered how stress is contagious at a cellular level.
A 2018 study (18) found that stress transmitted from someone else can change your brain in the same way that “real stress” (stress that you are exposed to) does. Corticotrophin-releasing hormone (CRH) neurons in the hypothalamus are activated when we perceive stress, and the researchers discovered that the activation of these CRH neurons in mice triggers the release of an “alarm pheromone” that chemically signals a non-stressed mouse nearby. Remarkably, this chemical signal activated CRH neurons in the non-stressed mice in the same way as in the mice that were exposed to stress.
This automatic way of communicating and responding to stress likely helps various species survive in groups; the member who detects the threat can silently alert other members of the group. But in human relationships today, it most often serves to increase the unnecessary stress we experience.
And it turns out that you don’t even need to be physically close to someone in order to be affected by their stress. Researchers found (19) that merely observing stressed people on video makes us release the stress hormone cortisol. This finding suggests that watching stressful television shows on a regular basis is likely not good for our stress level. On a larger scale, it speaks to the rising level of stress-related health conditions in the world and suggests that we might experience stress in response to observing any stressed person in any manner, like on the street or via the internet. Stress is literally contagious, and we are all more connected than ever before.
Even our pets are affected by our stress levels. A 2019 study (20) found that owners with high levels of cortisol have dogs with high levels of cortisol, and owners with low levels of cortisol have dogs with low levels. Based on the study’s assessment of the owners’ and dogs’ personalities, the researchers determined that dogs mirror their owner’s stress, and not the other way around.
In Conclusion
While we don’t know everything there is to know about the negative effects of chronic psychological stress, what we do know is enough to put reducing stress right up there with exercise and a healthy diet when it comes to health and longevity. Taking time to relax can feel selfish, indulgent, and unnecessary—but the more research you read on this topic, the more you’ll feel compelled to build relaxation—including yoga and meditation practice—and self-care into your daily routine. Reducing your stress level and changing your automatic reactions to stress will immediately improve your relationships, too. Try it and see!
Reprinted with permission from Somatic Movement Center.
 Sarah Warren St. Pierre is a Certified Clinical Somatic Educator and the author of the book Why We’re In Pain. She was trained and certified at Somatic Systems Institute in Northampton, MA. Sarah has helped people with chronic muscle, and joint pain, sciatica, scoliosis, and other musculoskeletal conditions become pain-free by practicing Thomas Hanna’s groundbreaking method of Clinical Somatic Education. Sarah is passionate about empowering people to relieve their pain, improve their posture and movement, and prevent recurring injuries and physical degeneration.
Sarah Warren St. Pierre is a Certified Clinical Somatic Educator and the author of the book Why We’re In Pain. She was trained and certified at Somatic Systems Institute in Northampton, MA. Sarah has helped people with chronic muscle, and joint pain, sciatica, scoliosis, and other musculoskeletal conditions become pain-free by practicing Thomas Hanna’s groundbreaking method of Clinical Somatic Education. Sarah is passionate about empowering people to relieve their pain, improve their posture and movement, and prevent recurring injuries and physical degeneration.
Recommended Reading:
-
The Pain Relief Secret: How to Retrain Your Nervous System, Heal Your Body, and Overcome Chronic Pain by Sarah Warren, CSE
-
Somatics: Reawakening the Mind’s Control of Movement, Flexibility and Health by Thomas Hanna
Resources
1. Picard, M., & McEwen, B. S. (2018). Psychological Stress and Mitochondria: A Systematic Review. Psychosomatic medicine,
80(2), 141–153. doi:10.1097/PSY.0000000000000545; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5901654/
2. https://www.cell.com/neuron/fulltext/S0896-6273(19)30487-8
3. Stress, GCR, inflammation, and disease risk Sheldon Cohen, Denise Janicki-Deverts, William J. Doyle, Gregory E. Miller, Ellen Frank, Bruce S. Rabin, Ronald B. Turner
Proceedings of the National Academy of Sciences Apr 2012, 109 (16) 5995-5999; DOI: 10.1073/pnas.1118355109
4. https://www.forbes.com/sites/daviddisalvo/2019/07/26/stress-changes-the-brain-and-this-could-be-how-it-happens/#20dffc0130d5
5. https://www.cell.com/neuron/fulltext/S0896-6273(19)30487-8
6. https://news.uthscsa.edu/study-stress-can-impair-memory-reduce-brain-size-in-middle-age/
7. Ansell, E. B., Rando, K., Tuit, K., Guarnaccia, J., & Sinha, R. (2012). Cumulative adversity and smaller gray matter volume in medial prefrontal, anterior cingulate, and insula regions. Biological psychiatry, 72(1), 57–64. doi:10.1016/j.biopsych.2011.11.022; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5901654/
8. http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.326.7670&rep=rep1&type=pdf
9. Justice N. J. (2018). The relationship between stress and Alzheimer’s disease. Neurobiology of stress, 8, 127–133. doi:10.1016/j.ynstr.2018.04.002 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5991350/
10. Zotova, E., Nicoll, J. A., Kalaria, R., Holmes, C., & Boche, D. (2010). Inflammation in Alzheimer’s disease: relevance to pathogenesis and therapy. Alzheimer’s research & therapy, 2(1), 1. doi:10.1186/alzrt24; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2874260/
11. https://www.hsph.harvard.edu/nutritionsource/microbiome/
12. https://www.ncbi.nlm.nih.gov/pubmed/11910364
13. Social-Stress-Responsive Microbiota Induces Stimulation of Self-Reactive Effector T Helper Cell, Michal Werbner, Yiftah Barsheshet, Nir Werbner, Mor Zigdon, Itamar Averbuch, Oren Ziv, Boris Brant, Evan Elliott, Shachaf Gelberg, Moran Titelbaum, Omry Koren, Orly Avnim Systems May 2019, 4 (4) e00292-18; DOI: 10.1128/mSystems.00292-18
14. Karl, J. P., Hatch, A. M., Arcidiacono, S. M., Pearce, S. C., Pantoja-Feliciano, I. G., Doherty, L. A., & Soares, J. W. (2018). Effects of Psychological, Environmental and Physical Stressors on the Gut Microbiota. Frontiers in microbiology, 9, 2013. doi:10.3389/fmicb.2018.02013; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6143810/
15. https://medicine.uq.edu.au/article/2017/11/researchers-show-stress-suppresses-response-cancer-treatments
16. https://www.nature.com/articles/s41586-019-1019-4
17. https://www.sciencedaily.com/releases/2019/03/190313143238.htm
18. https://www.nature.com/articles/s41593-017-0044-6
19. https://www.sciencedaily.com/releases/2014/04/140430133143.htm
20. https://www.sciencedaily.com/releases/2019/06/190606102036.htm
