Your Brain on Pain: How to Remap Your Brain and Reverse the Effects of Chronic Pain

Have you ever been told your pain is “all in your head?” Unfortunately, this is often the experience of many people experiencing persistent pelvic pain. Interestingly enough, the brain itself is actually very involved in producing pain, particularly when a person has experienced pain for a long period of time. Let’s explore how someone can come to have pain that is ingrained in their brain, literally, and more importantly, what we can do to help them get better.
Our brains are incredible, constantly changing and adapting; every second your brain fine-tunes connections between brain cells, called neurons, reflecting your everyday experiences. This works like a bunch of wires that can connect to one another in different pathways and can be rerouted. Another way to say this is “neurons that fire together, wire together.” This process of learning and adapting to experiences is known as neuroplasticity or neural plasticity. It is a well-documented occurrence in humans and animals. (1)
The brain has distinct physical areas that have been found to relate to different functions and parts of the body.
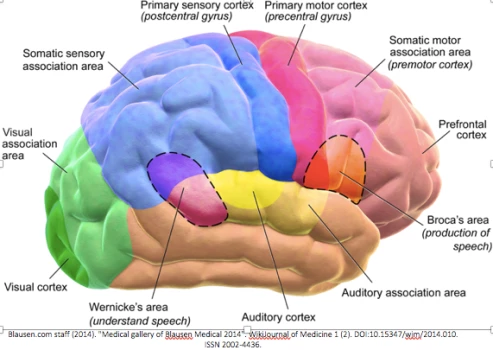
Those two spots in the middle that read “primary motor cortex” and “primary sensory cortex” relate to the control of body movements, and the interpretation of stimuli as sensations like hot, cold, sharp, or dull. “Interpretation” means the brain uses this area to make sense of the signals it’s receiving from the rest of the body and decides what this feels like. These areas can be broken down by body structure, too.
The Brain Map
This next image, is the brain cut down the middle, looking from the back of someone’s head to the front. This image illustrates the physical areas of the brain that correlate to specific limbs and body parts. This representation is known as a homunculus.
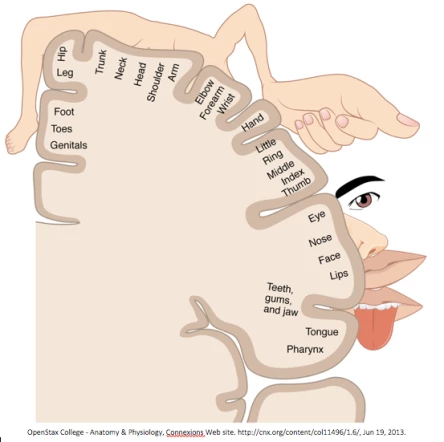
See how the hand and facial features look massive? That’s because we do a lot with our hands, have delicate control of our facial expressions, and feel many textures with both. Thus, these areas need a lot of physical space in our brains.
In this image, the pelvis takes up less space than other areas, but for people who pay a lot of attention to their pelvis, this area may be mapped differently, or may not be as well-defined. We know that the brain changes due to experiences, and ordinarily, it has a distinct physical map of structures. But what happens when that brain map is drawn differently with experiences like pain?
How Pain Can Change Our Brain Map
Studies suggest that over time, the brain undergoes changes related to long-lasting pain. If someone often has to pay attention to an area that is painful, they may experience changes in how their brain maps that experience on a day-to-day basis. This varies from person to person, and we’re still learning how this happens.
Here’s an example: in a recent study, people experiencing longstanding pelvic pain were found to have more connections in their brains than in those of a pain-free control group, among other findings. The greater the area of pain, the more brain changes were found. (2) This is an example of how the brain can undergo changes with pain, and can help explain how strange and scary it can feel for some.
How Pain Develops
The process that makes pain occur is complex. It often starts with some injury, surgery, or other experience causing tissue stress. First, cells respond by alerting nerves in the tissues. Then, that signal moves to the spinal cord and the brain, also called the central nervous system. The brain weighs the threat of the stress; neurons communicate with each other throughout the brain, in order to compare the stressor to prior experiences, environments, and emotions. The brain, the commander-in-chief, decides if it is dangerous, and responds with a protective signal in the form of pain.
Pain is a great alarm to make you change what you’re doing and move away from a perceived danger. Over time, however, the brain can over-interpret tissue stress signals as dangerous. Imagine an amplifier getting turned up on each danger signal, although the threat is still the same. This is how tissue stress can eventually lead to overly sensitive pain, even after the tissues themselves are healed. (3)
Additionally, your brain attempts to protect the area by smudging its drawing of the sensory and motor maps in a process called cortical remapping. Meaning, neurons have fired so much in an area that they rewire and connections spread out. This may be apparent if pain becomes more diffuse, spreads, and is harder to pinpoint or describe. For example, pain starts at the perineum or the tailbone, but over time is felt in a larger area, like the hips, back, or abdomen.
How Our Brains Can Create Pain
Pain alarms us to protect us, sometimes even when there’s nothing there! After having a limb amputated, people may feel as though the limb is still present and in pain. This is called phantom limb pain. The limb has changed, but the connections within the brain have not. However, over time the connections in the brain will reroute.
This example illustrates how the brain alone can create pain in an area. Pain does not equal tissue injury; the two can occur independently of one another. (4) Pain signals can also be created or amplified by thoughts, emotions, or beliefs regarding an injury. Has your pain ever gotten worse when you were stressed?
There is also some older case evidence that describes how chronic pain and bladder dysfunction evolved for people after surgery in a way that suggests this type of brain involvement. (5) Another case study describes a patient with phantom sensations of menstrual cramps following a total hysterectomy! (6)
Can We Change Connections That Have Already Been Remapped?
Yes!! The brain is always changing! There are clinicians who can help. Physicians have medications that target the central nervous system to influence how it functions. Psychologists and counselors can help people better understand their mental and emotional experiences as they relate to pain, and to work through these to promote health.
Physical therapy provides graded exposure to stimuli such as movement or touch, in a therapeutic way that promotes brain changes and improved tolerance to those stimuli that are painful. This can result in a clearer, well-defined brain map and danger signals that are appropriate for the actual level of threat. Physical therapists also help people improve their strength and range of motion, so they can move more, hurt less, and stay strong when life throws heavy things at us!
It is extremely important to return to moving normally and getting back to living! Poor movement strategies can prolong pain and dysfunction, and this can turn a short-term stressor into long-lasting, sensitized pain. In addition to physical therapy, yoga practice can teach us how to relearn healthy movement patterns.
Of course, with any kind of treatment, it also depends on the unique individual. Everyone has personal experiences associated with pain that can make treatment different for them. We are still learning about how neural plasticity occurs, but the brain does change. This is how we are all able to adapt to new environments and circumstances around us!
Pain is our protective mechanism, but sometimes it can get out of hand. While tissue injury can elicit pain, the nervous system can become overly sensitized to stimulus and cause pain with no real danger. This perception can spread beyond the original problem areas, and this can occur from connections remapping in the brain and the spinal cord. For pelvic pain, treatment is often multidisciplinary, but should include a pelvic health physical therapist who can facilitate tissue healing, optimal movement, and who can utilize the principles of neural plasticity to promote brain changes and return to function.
Yoga for Pain Relief: Yoga Offers Effective Relief for Back Pain, Fibromyalgia and Chronic Pain Issues Study Finds – another article from YogaUOnline and B. Grace Bullock, Ph.D.
Yoga for Back Pain: Keys to Safely Preventing and Relieving Back Pain – A YogaUOnline pain relief course with Dr. Loren Fishman and Ellen Saltonstall.
Reprinted with permission from Jessica Reale PT Blog
 Amanda Bastien is a graduate student at Emory University in Atlanta, GA, currently completing her Doctorate of Physical Therapy degree, graduating in May 2018. Amanda has a strong interest in pelvic health, orthopedics, neuroscience and providing quality information and care to her patients.
Amanda Bastien is a graduate student at Emory University in Atlanta, GA, currently completing her Doctorate of Physical Therapy degree, graduating in May 2018. Amanda has a strong interest in pelvic health, orthopedics, neuroscience and providing quality information and care to her patients.
References:
(1) Kleim, J.A., Jones, T.A. (2008). Principles of experience-dependent neural plasticity: Implications for rehabilitation after brain damage. Journal of Speech, Language, and Hearing Research, 51, S225-S239. Retrieved from: https://www.jsmf.org/meetings/2008/may/Kleim%20&%20Jones%202008.pdf
(2) Kutch, J. J., Ichesco, E., Hampson, J. P., et al. (2017). Brain signature and functional impact of centralized pain: a multidisciplinary approach to the study of chronic pelvic pain (MAPP) network study. PAIN, 158, 1979-1991.
(3) Origoni, M., Maggiore, U. L. R., Salvatore, S., Candiani, M. (2014). Neurobiological mechanisms of pelvic pain. BioMed Research International, 2014, 1-9. http://dx.doi.org/10.1155/2014/903848
(4) Flor, H., Elbert, T., Knecht, S. et al. (1995). Phantom -limb pain as a perceptual correlate of cortical reorganization following an arm amputation. Nature, 375, 482-484.
(5) Zermann, D., Ishigooka, M., Doggweiler, R., Schmidt, R. (1998) Postoperative chronic pain and bladder dysfunction: Windup and neuronal plasticity – do we need a more neurological approach in pelvic surgery? Urological Neurology and Urodynamics, 160, 102-105.
(6) Dorpat, T.L. (1971) Phantom sensations of internal organs. Comprehensive Psychiatry, 12(1), 27-35.
